OSUmetstud
Meteorologist-
Posts
16,521 -
Joined
-
Last visited
Content Type
Profiles
Blogs
Forums
American Weather
Media Demo
Store
Gallery
Everything posted by OSUmetstud
-
Federally mask mandate is a non starter. Asking cops to enforce mask wearing especially in minority communities is just asking for trouble. The essential problem has always been the lack of leadership and the administration undermining public health and general science. CDC needs to be taking the front role and working with state health departments.
-
Standard for data from conservatives in 2020: "I saw a lot of out of state hats"
-
What is it? Are we over it? Or are we taking it seriously? Blaming the southern spread in June/July/August on tourism is silly.
-
It is real. But the majority of people still care about this and are following public health guidance. Follow the conversation.
-
It seems like you're the one who wanted to makes it political. Cool.
-
This doesn't support your assertion that the "majority of people are over caring about this" if the Rt is well under the Ro if the virus.
-
Some fatigue doesn't mean the majority of people stopped caring.
-
The data just doesn't support people are living their lives completely normally. Mobility data is well below baseline and mask use has come up generally. It's why there isn't 500k cases and 1000 and 1000s of covid deaths a day. https://covid19.healthdata.org/united-states-of-america?view=social-distancing&tab=trend
-
You saying this doesn't make it true. We would be seeing far more rapid spread (close to Ro) if the majority of people weren't following public health guidance.
-
Don't worry its a La Nina so the MA and the SE will be warm and snowless.
-
Sounds like Judah needs help.
-
I think its increased death reporting delay...but I don't know for sure.
-
Decent mask study (This is peer reviewed/published) A cotton mask led to an approximately 20% to 40% reduction in virus uptake compared to no mask In contrast, when a mask was attached to the mannequin that released virus, cotton and surgical masks blocked more than 50% of the virus transmission, whereas the N95 mask showed considerable protective efficacy (Fig. 2C). There was a synergistic effect when both the virus receiver and virus spreader wore masks (cotton masks or surgical masks) to prevent the transmission of infective droplets/aerosols (Fig. 2D and E). https://msphere.asm.org/content/5/5/e00637-20#F2
-
From a hospitalizations standpoint, the wave in the UK is about 1/3rd as bad so far as the early April wave. There were close to 20k people in hospital then, now there about 6500.
-
Lol @ hamstering
-
I don't buy that most people are being selfish and unreasonable. If they were, the pandemic would be raging completely out of control with 1000s of deaths a day. The transmission rate doesn't suggest that most people are acting like that. They are just a very loud minority.
-
I think at this point, unless it gets crazy bad, targeted restrictions have shown to work (like closing bars and large, indoor events, and reducing restaurant capacity. I think you need to have regional-type lockdowns in your bag of tricks for the coming winter in case things go really sideways and hospitals are on the verge of getting overwhelmed.
-
Only about 10% of the US has been infected. And all the information for vaccine development has been quite favorable...we might be only months away from widespread implementation (early 2021). It will only infect everyone if the vaccine took a few more years to develop imo. If it's here in the Spring, herd immunity will not have to be achieved through natural infection. Besides, there are advantages to slowing down infection, like better treatments, and less overwhelmed hospitals. So restrictions do prevent covid deaths.
-
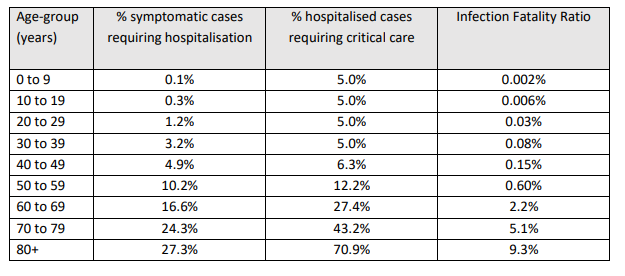
The CDC estimates a population level IFR of about 0.9 percent and about 10% infected so far. https://www.google.com/amp/s/www.cnbc.com/amp/2020/09/23/cdc-director-says-more-than-90percent-of-americans-remain-susceptible-to-the-coronavirus.html https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html
-
Upstate NY Banter and General Discussion..
OSUmetstud replied to wolfie09's topic in Upstate New York/Pennsylvania
Yeah, interesting technology for sure. -
Agreed on the flu, it's more likely to be mild given what the southern hemisphere observed. Eh. Not sure about this. We missed a ton of infections in the very beginning of the pandemic, so much so that there were maybe like 500K infections per day at the peak in early April in the US. We are catching a way higher proportion of infections now, so the ratio of cases-hospitalizations-deaths appears much higher. Most people are being fairly careful, especially so when they see an outbreak in their community and then take further action, which can drive the Rt back to near or under 1.
-
Upstate NY Banter and General Discussion..
OSUmetstud replied to wolfie09's topic in Upstate New York/Pennsylvania
They're scenarios. I think that's important to appreciate. But, when I saw the first best guess one they posted at 0.26 (I think it was April?), I was pretty skeptical. It seemed very low given the American experience thus far. They did a July update to 0.65, and then this one on September 10th to the banded age groups. It's actually quite close to the imo wrongly maligned University of College London study from March 16th which had an age banded 0.9% and projected the 2.2 million US deaths in an unmitigated pandemic. I don't think we've ever tried to make a coronavirus vaccine, at least to this great extent. We're throwing all the will and might of science and cash at the problem. They were getting close with SARS (and they are using some of that research/technology for this one), but then because it is only infectious when people are very sick, we were able to isolate everyone and the infection died out so we didn't need it. I think the most likely scenario is that the vaccine reduces severe disease but doesn't prevent infection and that SARS-Cov 2 becomes a fairly benign endemic seasonal coronavirus in the next several years much like the other ones. -
This report provides preliminary evidence that younger adults contributed to community transmission of COVID-19 to older adults. Across the southern United States in June 2020, the increase in SARS-CoV-2 infection among younger adults preceded the increase among older adults by 4–15 days (or approximately one to three incubation periods). Similar observations have been reported by the World Health Organization.*** Further investigation of community transmission dynamics across age groups to identify factors that might be driving infection among younger adults and subsequent transmission to older adults is warranted. These findings have important clinical and public health implications. First, occupational and behavioral factors might put younger adults at higher risk for exposure to SARS-CoV-2. Younger adults make up a large proportion of workers in frontline occupations (e.g., retail stores, public transit, child care, and social services) and highly exposed industries (e.g., restaurants/bars, entertainment, and personal services) (4,5), where consistent implementation of prevention strategies might be difficult or not possible. In addition, younger adults might also be less likely to follow community mitigation strategies, such as social distancing and avoiding group gatherings (6,7). Second, younger adults, who are more likely to have mild or no symptoms,††† can unknowingly contribute to presymptomatic or asymptomatic transmission to others (2), including to persons at higher risk for severe illness. Finally, SARS-CoV-2 infection is not benign in younger adults, especially among those with underlying medical conditions,§§§ who are at risk for hospitalization, severe illness, and death (8). Increased prevalence of SARS-CoV-2 infection among younger adults likely contributes to community transmission of COVID-19, including to persons at higher risk for severe illness, such as older adults. Emphasis should be placed on targeted mitigation strategies to reduce infection and transmission among younger adults, including age-appropriate prevention messages (7), restricting in-person gatherings and events,**** recommending mask use and social distancing in settings where persons socialize,†††† implementing safe practices at on-site eating and drinking venues (9), and enforcing protection measures for essential and service industry workers.§§§§ Given the role of asymptomatic and presymptomatic transmission (2), all persons, including young adults, should take extra precautions to avoid transmission to family and community members who are older or who have underlying medical conditions. Strict adherence to community mitigation strategies and personal preventive behaviors by younger adults is needed to help reduce their risk for infection and minimize subsequent transmission of SARS-CoV-2 to persons at higher risk for severe COVID-19. https://www.cdc.gov/mmwr/volumes/69/wr/mm6939e1.htm#F1_down
-
Upstate NY Banter and General Discussion..
OSUmetstud replied to wolfie09's topic in Upstate New York/Pennsylvania
https://www.cnbc.com/2020/09/23/cdc-director-says-more-than-90percent-of-americans-remain-susceptible-to-the-coronavirus.html#:~:text=Health and Science-,CDC director says more than 90% of,remain susceptible to the coronavirus&text=“A majority of our nation,of Americans are still susceptible.” Per the national lab survey data from August 15th, it does appear that older Americans are doing a reasonable job in shielding themselves. Their seroprevalence is considerably lower than the younger cohorts. https://covid.cdc.gov/covid-data-tracker/#national-lab -
Upstate NY Banter and General Discussion..
OSUmetstud replied to wolfie09's topic in Upstate New York/Pennsylvania
Across countries, model estimates of IFR ranged from 0.5% (95% CrI 0.4%–0.6%) in Switzerland to 1.4% (95% CrI 1.1%–1.6%) in Lombardy, Italy. The patterns of age-specific IFR estimates were similar across locations (Fig 4B), despite differences in the surveillance-reported age distribution of cases The IFR increased with age; among those 80 years or older, estimates ranged from 20% in Switzerland to 34% in Spain.